Deciding to Have Sex
Several things may impact a person’s decision about when to have sex:
- Choosing the Right Person: You may have certain standards about a person with whom you would consider having sex. You might want to feel respect, trust, or love before having sex.
- Choosing the Right Time: Perhaps school is too stressful, you’re still dealing with a bad break-up, or you’re just not ready for a variety of personal reasons. Maybe you want to wait until you’re in a serious, committed relationship or married.
- Choosing the right circumstances: You might not want to have sex in specific circumstances for a variety of reasons; maybe you’re tired, have had too much to drink, or aren’t ready to go there yet with a particular partner.
Communication With Your Partner & Consent
It isn't always easy navigating the discussion of sex with your partner. Here are few scenarios that might help you with your preference of approach:
-
What is consent?
-
When someone doesn't want to to have sex:
-
When someone isn't sure about having sex:
-
When someone definitely wants to have sex:
Risk Reduction Tips & Information
The only way to protect one’s self from Sexually Transmitted Infections (STIs) and an unplanned pregnancy is to abstain from sexual intercourse (oral, vaginal, anal). If it is not realistic for an individual to abstain, then they can reduce their risk of an unplanned pregnancy and/or contracting or transmitting an STI. Many of your safer sex and risk reduction questions are answered below.
What is the ‘continuum of risk’?
This refers to all types of sexual activity, including oral, vaginal and anal sex, in which the risk associated with each type of sexual activity and whether or not a barrier is used is on a continuum. In general, risk for STIs is associated with all forms of sexual activity; however, unprotected oral sex is the least risky followed by unprotected vaginal sex followed by unprotected anal sex
Because only blood, semen, breast milk and vaginal secretions can transmit infection, using a barrier for any of these sex acts reduces one’s risks of STIs (i.e., anal sex with a barrier is less risky than unprotected vaginal sex).
What exactly is ‘safer sex’?
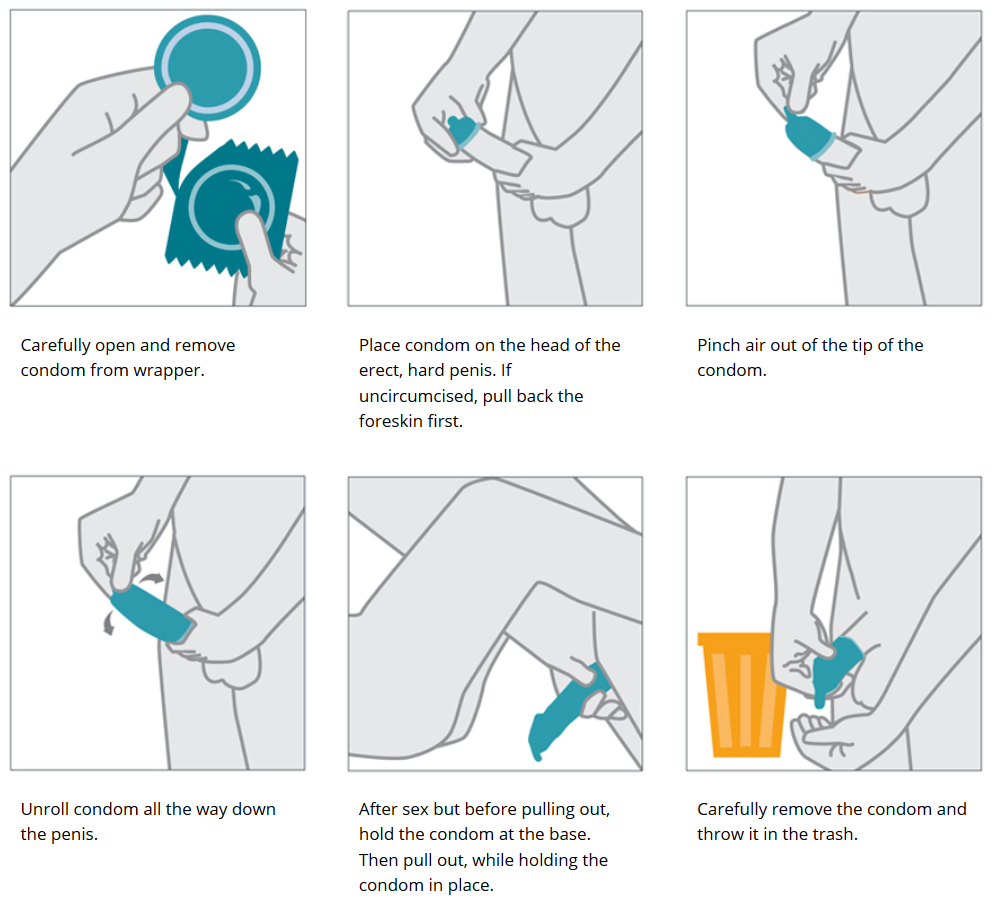
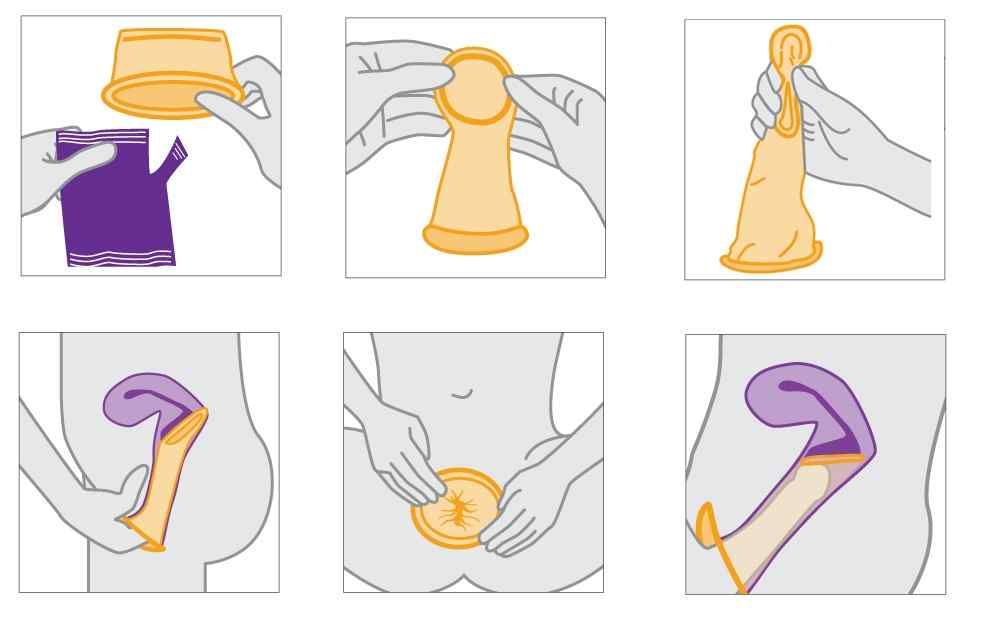
Safer sex refers to using a barrier method (condom, female condom, dental dam) to reduce the risk of bodily fluid transmission between partners. By practicing safer sex, you show concern and respect for your partner and yourself, as well as allow yourself to enjoy sex without acquiring or transmitting STIs.
Is there such a thing as ‘safe sex’?
No. There is no 100% safe sex as there is always the risk of STI transmission and/or unplanned pregnancy. However, you can make sex safer by using barrier methods as discussed below.
What is Abstinence?
Abstinence often means different things to different people, so it is important to know what your definition is and what risk may be involved when following your definition. Typically, abstinence means that there is no chance for bodily fluids to exchange (semen, vaginal secretions, or blood) between partners. It is also a good idea to know where you stand regarding sexual activity before you become physically intimate with someone.
Can I be abstinent if I have had sex before?
Yes! Abstinence is a choice that can be made for a lifetime, months, days, or even for a night. It may mean simply waiting until you find the right person to have sex with, or the right time and place. You can always choose abstinence.
How many partners does the typical MSU student have?
The majority of Michigan State University students have had no, or just one, sexual partner in the last year (including oral, anal, and vaginal sex partners):
30% of MSU students reported having no sexual partners on the last year*
47% of MSU students reported having one sexual partner in the last year*
Why do people choose NOT to have sex?
People abstain from sex for many reasons – even after they’ve been sexually active. Some of these reasons include:
- Waiting until they’re ready for a sexual relationship
- Waiting to find the “right” partner
- Getting over a breakup
- Wanting to avoid pregnancies or STIs
- Having fun with friends without sexual involvement
- Pursuing academic, career, or extracurricular activities
- Supporting personal, cultural, or religious values
- Following medical advice during an illness or infection.
Tips for sticking with your decision NOT to have sex:
- Plan ahead so you know how you’ll handle potentially tricky situations.
- Remember that alcohol and other drugs can impair your judgment.
- Try to find supportive people in your life to talk to about your decision.
- Think about how you could talk to a current or future partner about your decision.
- Don’t reevaluate your decision not to have sex when you’re in a sexual situation.
- Stay with your decision until you can think about it with a clear head. When you do choose to have sex, be sure that you know how to protect yourself from STIs and unintended pregnancy.
Is masturbation harmful?
Masturbation is actually very healthy as it helps to relieve sexual tension and stress, and when done alone, there is no risk for STI transmission or an unplanned pregnancy. Masturbation is a very personal issue, as some people choose to masturbate often, some choose to masturbate infrequently and others choose not to masturbate at all. How often one chooses to masturbate is perfectly fine as long as that person is comfortable. Masturbation becomes "harmful" if it starts to interfere with your daily life, activities and/or relationships with others (friends, family, partners, etc.), and/or if it is painful to you.
Where is the clitoris?
The clitoris, a small external female organ that is highly sensitive, is located above the opening of the urethra (the structure urine comes out of) and the vagina.
What is the "G-spot"?
There is some controversy surrounding this issue, some say it exists and others say that it does not exist. For those researchers (and others) who believe it exists, it is called the Grafenberg spot, or G-spot for short. It is located on the top side of the vagina, about half way between the pubic bone and cervix, when a female is lying down on her back. When this spot is stroked, there is a sensation or urge to urinate, but if the stroking is continued for a little while longer (a few seconds), it can be sexually pleasurable for females (Shibley Hyde, J. and DeLamater, J.D., Understanding Human Sexuality, Eighth Edition (2003)).
Is ejaculation the same thing as an orgasm?
No. Ejaculation is the release of semen from the penis; whereas, orgasm is a series of muscle contractions that release sexual tension and is usually very pleasurable. Although ejaculation usually occurs during orgasm, it does not have to (i.e., one can ejaculate without orgasm and one can orgasm without ejaculation). This is similar for female ejaculation as well.